- Cataract eye surgery is a common and effective procedure used to treat cataracts, a condition characterised by the clouding of the eye’s natural lens. The Aim of surgery is to remove the clouded lenses and change them with a fake intraocular lens (IOL) to restore crystal-clear vision. here are several facts about cataract surgery in paragraphs:
- Cataract surgery is usually an outpatient procedure perform by an ophthalmologist, a specialist in eye surgery. It is usually done under local anaesthetic, which numbs the eye area and allows the patient to remain awake during the procedure. In some cases, general anaesthetic may be use, especially if the patient is unable to cooperate or has other medical conditions.
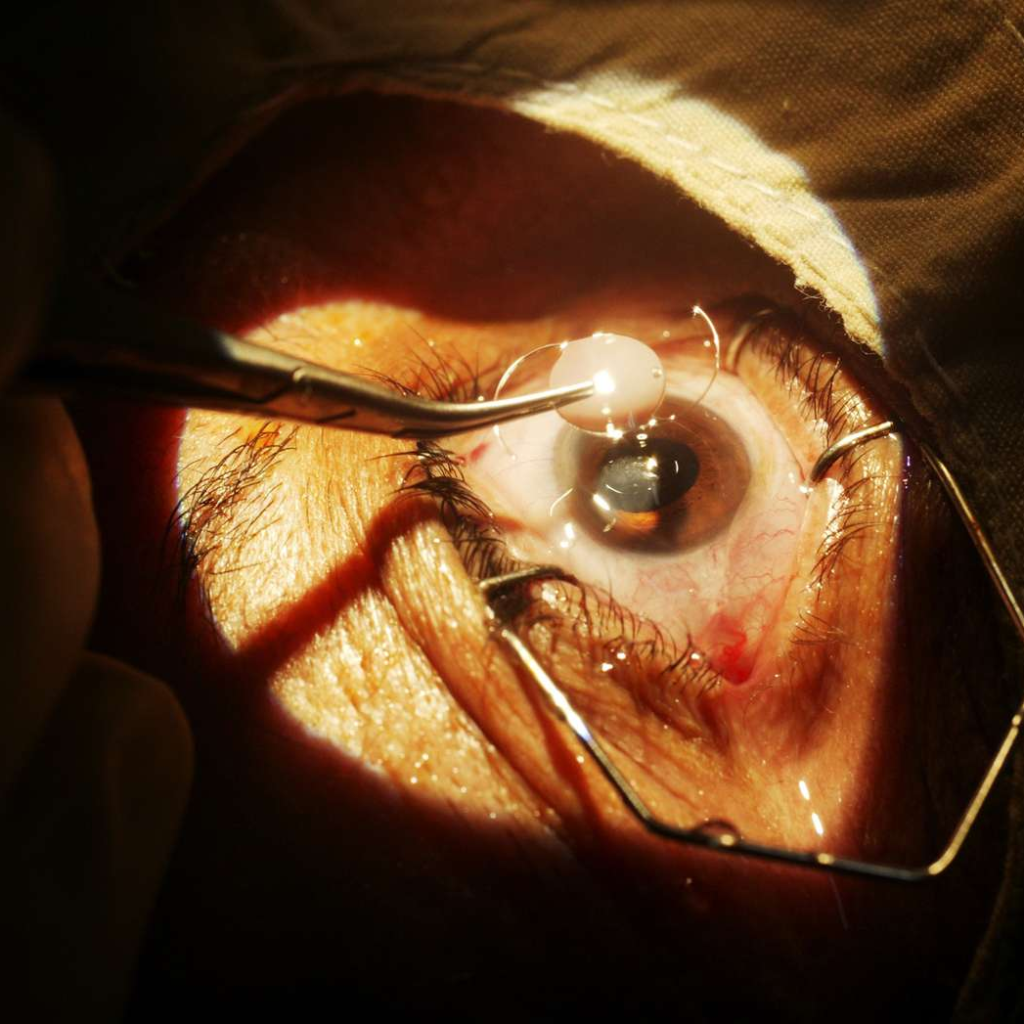
- During the operation, the surgeon makes a small incision in the cornea, the clear front part of the eye. The cloudy lens is then gently broken up and removed from the eye using various techniques, such as phacoemulsification. Once the cataract is removed, an artificial IOL is implanted in its place to restore clear vision. The IOL is chosen based on the patient’s visual needs and there are several types of cataract available, including monofocal, multifocal and toric lenses.
- Cataract surgery is a relatively quick procedure, usually lasting between 15 and 30 minutes. After the operation, the patient may spend a short time in a recovery room for observation before being discharged. Most patients can go home the same day and resume normal activities within a few days, although specific post-operative instructions given by the surgeon should follow for optimal healing.
Types of Cataract Surgery
Here are some Types of Cataract
- Phacoemulsification: Phacoemulsification, often called “phaco”, is the most common and widely used technique for cataract surgery. It involves making a small incision in the cornea, the clear front part of the eye, and inserting a tiny probe. The probe uses ultrasound waves to break up the cloudy lens into small fragments, which are then gently suck out. Phacoemulsification has several advantages, including a smaller incision, faster recovery and a lower risk of complications.
- Extracapsular cataract extraction (ECCE): Extracapsular cataract extraction is an older technique that may be use in certain cases when phacoemulsification is not possible or appropriate. With ECCE, a larger incision is made in the cornea or sclera (white part of the eye) to remove the cloudy lens in one piece, leaving the posterior part of the lens capsule intact. The artificial IOL is then insert into the remaining lens capsule. This technique requires more stitches and may involve a longer recovery period than phacoemulsification.
- Femtosecond laser-assisted cataract surgery (FLACS): Femtosecond laser-assisted cataract surgery is a newer technique that uses laser technology to perform key steps of the procedure. FLACS uses a femtosecond laser to make precise incisions in the cornea, softening the cataract and breaking it into fragments. This makes it easier to remove the cataract and insert the IOL. FLACS offers improved accuracy, customisation and potentially faster visual recovery. However, it may not be available or suitable for all patients due to factors such as cost or specific eye conditions. these are the three types of Cataract gave above.
Causes of Cataract Eye Surgery
- Age: Age is the main risk factor for developing cataracts. As we age, the proteins in the lens of the eye can begin to clump together, causing the lens to become cloudy and opaque. This gradual process eventually affects vision and may require surgery.
- Genetics: Certain genetic factors may predispose people to cataracts. If you have a family history of cataracts, you may have a higher risk of developing them and may need cataract eye surgery at some point in your life.
- Trauma or injury: Major eye trauma or injury can cause cataracts to develop, sometimes requiring surgical removal. Blunt force trauma, penetrating injuries or exposure to intense radiation can damage the lens and lead to cataract formation.
- Medications and medical conditions: Prolonged use of certain medications, such as corticosteroids or certain types of eye drops, can increase the risk of cataracts. In addition, certain medical conditions such as diabetes, high blood pressure or long-term exposure to ultraviolet (UV) radiation can contribute to the development of cataracts and the need for surgery.
- Lifestyle factors: Certain lifestyle choices can influence the development and progression of cataracts. Factors such as smoking, excessive alcohol consumption, poor diet and prolonged exposure to sunlight without protective eyewear may increase the risk of cataracts and require surgical treatment.
- Congenital or birth-related causes: In some cases, babies are born with cataracts or develop them shortly after birth. These congenital cataracts may require surgery to restore or maintain vision.
What happens during Cataract Eye Surgery?
- Cataract surgery removes the cloudy lens of the eye and replaces it with an artificial intraocular lens (IOL). It is usually do as an outpatient procedure under local anaesthetic. Here’s a general overview of what happens during cataract surgery:
- Preparation: Before surgery, the eye is numb with a local anaesthetic, which may give as eye drops or injected around the eye. You may also be give a sedative to help you relax during the operation. The surgical team will clean the area around your eye and place a sterile drape over your face, leaving the surgical site exposed.
- Incision: The surgeon will make a small incision in the cornea, the clear front part of the eye. The incision is usually about 2 to 3 millimetres long and is made using a precise surgical blade or a femtosecond laser.
- Capsulotomy: A circular opening is made in the front of the lens capsule, a thin, transparent membrane that holds the natural lens in place. This allows access to the clouded lens inside.
- Removing the lens: There are different techniques for removing the cataract, depending on the surgical approach used. The most common technique is to call phacoemulsification. Phacoemulsification involves inserting a small ultrasound probe through the incision. The probe uses high-frequency sound waves to break up the cloudy lens into tiny fragments, which are then gently sucked out through the probe. Some surgeons may also use a laser or other methods to break up and remove the cataract.
- Closure: Once the IOL is correctly position, the surgeon ensures that it is stable and centred. The incision is usually self-sealing and does not require stitches in most cases. The eye may be gently irrigate with a saline solution to remove any remaining debris or particles.
Risks of Cataract Surgery
- Infection: Infection is a rare but serious complication of any surgery, including cataract surgery. Precautions are taken to minimise the risk of infection, such as using sterile techniques and prescribing antibiotic eye drops before and after surgery. However, there is still a small chance of developing an infection that may require additional treatment.
- Bleeding: There is a small risk of bleeding inside the eye during cataract surgery. Although rare, excessive bleeding can potentially cause vision problems and may require additional procedures to control the bleeding.
- Swelling or inflammation: Inflammation may occur after cataract surgery, causing swelling of the eye tissues. This condition is to call postoperative inflammation or uveitis. Most cases of inflammation can treat with steroid eye drops or other medications. However, severe inflammation may require additional treatments or prolonged use of medication.
- Retinal detachment: Although rare, there is a small risk of retinal detachment after cataract surgery. Retinal detachment occurs when the light-sensitive layer at the back of the eye separates from the underlying supporting tissue. Symptoms may include a sudden increase in floaters, flashes of light or a curtain-like shadow in the peripheral vision. Retinal detachment requires immediate medical attention and surgical repair to prevent permanent vision loss.
- Dislocated intraocular lens (IOL): In rare cases, the implanted IOL may shift or dislocate after cataract surgery. This can cause vision problems and may require additional surgery to reposition or replace the IOL.
- Posterior capsule opacification (PCO): PCO is a clouding of the posterior part of the lens capsule that can occur months or years after cataract surgery. It can cause blurred or hazy vision, similar to the symptoms of a cataract. PCO can be easily treat with a quick and painless laser procedure called “YAG laser capsulotomy” to clear the visual axis.
After Cataract Surgery
- Post-operative care: Your ophthalmologist will give you specific post-operative instructions to follow. This may include the use of prescribed eye drops to prevent infection, reduce inflammation and promote healing. It’s important to use the eye drops as directed and according to the recommended schedule.
- Protective eyewear: You may be advise to wear a protective shield or glasses to protect your eyes from accidental injury or rubbing during the initial recovery period. It’s important to protect your eyes from any potential trauma or pressure.
- Rest and recovery: It’s normal to experience some mild discomfort, itching or irritation in the operated eye(s) immediately after surgery. Resting and avoiding strenuous activity for a few days may help to promote healing and reduce the risk of complications. You may also be advise to avoid activities that can increase eye pressure, such as heavy lifting or bending.
- Follow-up visits: Your ophthalmologist will schedule follow-up visits to monitor your healing and evaluate your vision. These visits allow your surgeon to check the incision site, assess the IOL position, and ensure that your eyes are healing properly. Attend all scheduled appointments and let your doctor know of any concerns or problems you may have.
- Medications and eye care Continue to use the prescribed eye drops as directed by your eye doctor. these drops help prevent infection, reduce inflammation, and speed healing. It is important to strictly adhere to the recommended dosage and duration of treatment. Avoid touching or rubbing your eyes and practice good hand hygiene to minimize the risk of infection.
- Sight correction: Although cataract surgery improves vision, you may still need vision correction for certain activities, such as reading or driving. Your optician can advise you on whether you need glasses or contact lenses for optimal vision.
Conclusion:
cataract eye surgery is a safe and effective procedure that can significantly improve vision and quality of life for individuals with cataracts and their are various types of cataract. By removing the cloudy lens and replacing it with a clear artificial lens, the surgery restores clear vision, allowing patients to see the world more vividly. With modern advancements and skilled surgeons, cataract surgery has become a routine outpatient procedure, ensuring quick recovery and minimal discomfort. If you’re experiencing vision problems due to cataracts, don’t hesitate to explore the benefits of cataract eye surgery and regain your clear sight today.
*Disclaimer: This article is for informational purposes only and should not substitute professional medical advice. Please consult a healthcare professional for a thorough evaluation of your symptoms and appropriate treatment.
