Varicose veins are a prevalent circulatory condition that affects a significant number of individuals worldwide. These enlarged and twisted veins, commonly found in the legs and feet, can cause discomfort and self-consciousness. In this comprehensive article, we will delve into the various aspects of varicose veins, including their causes, symptoms, and available treatment options. With our expertise in vascular health, we aim to provide you with valuable insights and practical advice to understand and manage this condition effectively.
Understanding Varicose Veins: Types and Causes
Varicose veins refer to enlarged, swollen veins that usually appear on the legs and feet. They occur when the one-way valves inside the veins malfunction, causing blood to accumulate and exert pressure on the vessel walls. Over time, this pressure weakens the veins, leading to their bulging and twisting appearance. There are two primary types of varicose veins:
- Superficial Varicose Veins: These are located just below the surface of the skin and are often visible as dark blue or purple bulging veins.
- Deep Varicose Veins: These affect the deeper veins in the leg muscles and may not be as visible but can cause significant discomfort.
Several factors contribute to the development of varicose veins, including:
- Age: Aging leads to wear and tear of veins, causing valves to weaken, increasing the risk of varicose veins.
- Gender: Women are more susceptible to varicose veins due to hormonal changes during pregnancy and menopause.
- Genetics: Family history plays a significant role in developing varicose veins, indicating a genetic predisposition.
- Prolonged sitting or standing: Occupations that involve long hours of sitting or standing impede blood circulation, contributing to vein dysfunction.
- Obesity: Excessive weight puts pressure on veins, hindering blood flow and leading to the development of varicosities.
- Pregnancy: Hormonal changes and increased blood volume during pregnancy strain the veins, increasing the likelihood of varicose veins.
- Lack of physical activity: Sedentary lifestyles contribute to poor circulation, weakening veins and promoting varicose veins.
- Smoking: Smoking damages blood vessels and reduces blood flow, elevating the risk of varicose veins.
- Deep vein thrombosis: A blood clot in deep veins can impede blood flow, causing varicose veins in the affected area.
- Previous leg injuries: Trauma to the legs, such as fractures or surgeries, can impair vein function and lead to varicose veins.
Identifying Symptoms and Possible Complications
Recognizing the symptoms of varicose veins is crucial for early intervention and effective management. Common signs and symptoms include:
- Visible veins: Varicose veins appear as enlarged, twisted, or bulging veins on the legs, often visible through the skin.
- Aching or heaviness: Individuals may experience discomfort or a feeling of heaviness in the legs, especially after prolonged periods of standing or sitting.
- Swelling: Varicose veins can cause swelling in the ankles and feet due to poor blood circulation.
- Leg cramps: Muscle cramps, particularly at night, are common symptoms of varicose veins.
- Itching or burning: Some individuals may experience itchiness or a burning sensation around the affected veins.
- Skin discoloration: Varicose veins can lead to skin discoloration, giving a darkened or discolored appearance in the affected area.
- Dry or thinning skin: The skin around varicose veins may become dry, fragile, or prone to developing ulcers.
While varicose veins are often harmless, they can lead to complications if left untreated. Potential illnesses associated with varicose veins include:
- Venous Ulcers: Chronic venous insufficiency resulting from untreated varicose veins can lead to the development of venous ulcers. These open sores on the skin are difficult to heal and can cause pain and discomfort.
- Thrombophlebitis: Varicose veins increase the risk of thrombophlebitis, which is inflammation of the veins caused by blood clots. This condition can lead to pain, redness, swelling, and potential complications if the clot travels to other parts of the body.
- Bleeding: Varicose veins close to the skin’s surface are more prone to injury. Even minor trauma or injury can result in bleeding, which may require medical attention.
- Superficial Thrombophlebitis: Inflammation of the superficial veins near the skin’s surface can occur due to varicose veins. Although generally not as serious as deep vein thrombosis, it can still cause discomfort, redness, and swelling.
- Hyperpigmentation: Varicose veins can cause the skin around them to become discolored, leading to hyperpigmentation. The affected area may appear dark or have a reddish-brown discoloration.
- Lipodermatosclerosis: In some cases, varicose veins can result in lipodermatosclerosis, a condition characterized by inflammation and hardening of the skin. This condition can cause pain, tightness, and changes in skin texture.

Varicose Veins in Children: Understanding the Condition and Its Impact
Varicose veins, commonly associated with adults, can also affect children, albeit less frequently. This circulatory condition, characterized by enlarged and twisted veins, can pose challenges for children’s physical comfort and self-esteem. In this informative article, we will explore varicose veins in children, including their causes, symptoms, and available treatment options. With our expertise in vascular health, we aim to provide valuable insights and practical guidance to help parents and caregivers understand and address this condition effectively.
Causes and Risk Factors for Varicose Veins in Children
While varicose veins in children are relatively uncommon, they can be caused by various factors. Congenital abnormalities in the veins, such as weak vein walls or defective valves, can contribute to the development of varicose veins from an early age. Additionally, genetic predisposition, hormonal imbalances, obesity, and prolonged periods of standing or sitting can increase the risk of varicose veins in children. Recognizing these causes and risk factors is essential for early intervention and appropriate management.
Identifying Symptoms and Addressing Concerns
Identifying symptoms of varicose veins in children is crucial for timely intervention. Common signs include visible veins that are enlarged, twisted, or protruding, discomfort or pain in the affected areas, swelling, and skin discoloration. While varicose veins in children may not always cause significant pain, they can still affect their confidence and overall well-being. Addressing these concerns and seeking medical advice is vital to ensure proper management and support.
Treatment Options for Children with Varicose Veins
Managing varicose veins in children often involves a multidisciplinary approach. Conservative measures such as regular exercise, leg elevation, and compression stockings may be recommended to improve blood circulation and alleviate symptoms. In some cases, minimally invasive procedures like sclerotherapy or laser therapy may be considered to address more severe or persistent varicose veins. Consulting with a healthcare professional specializing in pediatric vascular conditions is crucial to determine the most appropriate treatment plan for each child’s unique situation.
Conclusion: Empowering Parents and Caregivers with Knowledge and Support
While varicose veins in children are relatively uncommon, they can still present challenges that require attention and care. By understanding the causes, symptoms, and available treatment options, parents and caregivers can take proactive steps to manage varicose veins effectively in children. Seeking professional guidance and support is vital to ensure appropriate care and minimize the impact on the child’s physical and emotional well-being. Trustworthy information and expert advice can empower parents and caregivers to make informed decisions and provide the necessary support for children with varicose veins.
Natural Remedies to Treat Varicose Veins at Home
While medical interventions are available for severe cases, several natural remedies can help alleviate varicose veins’ symptoms and promote better blood circulation. It is important to note that these remedies may not eliminate varicose veins entirely but can provide relief. Some effective home remedies include:
- Exercise: Engaging in regular physical activity, such as walking, swimming, or cycling, helps improve blood flow and strengthen leg muscles. Aim for at least 30 minutes of exercise most days of the week.
- Compression stockings: Wearing compression stockings or socks can provide external support to the veins, reducing swelling and discomfort. These garments apply pressure to improve blood circulation.
- Leg elevation: Elevating the legs above heart level for short periods can help reduce swelling and improve blood flow. Lie down and prop your legs up on pillows or use a reclining chair.
- Dietary changes: Adopting a healthy, balanced diet can promote vascular health. Include foods rich in fiber, antioxidants, and flavonoids, such as fruits, vegetables, whole grains, and legumes.
- Weight management: Maintaining a healthy weight can reduce the strain on veins and improve blood circulation. Incorporate regular exercise and a balanced diet to achieve and maintain a healthy weight.
- Herbal remedies: Certain herbal supplements, such as horse chestnut extract, butcher’s broom, and grape seed extract, have shown potential in reducing inflammation and improving blood circulation. Consult with a healthcare professional before using any herbal remedies.
- Avoid prolonged sitting or standing: Take regular breaks if your occupation involves long periods of sitting or standing. Move around, stretch, and flex your leg muscles to improve blood circulation.
While these natural remedies can provide relief and support, it’s important to note that they may not eliminate varicose veins entirely. For severe cases or persistent symptoms, it’s advisable to consult a healthcare professional for a comprehensive evaluation and personalized treatment plan.
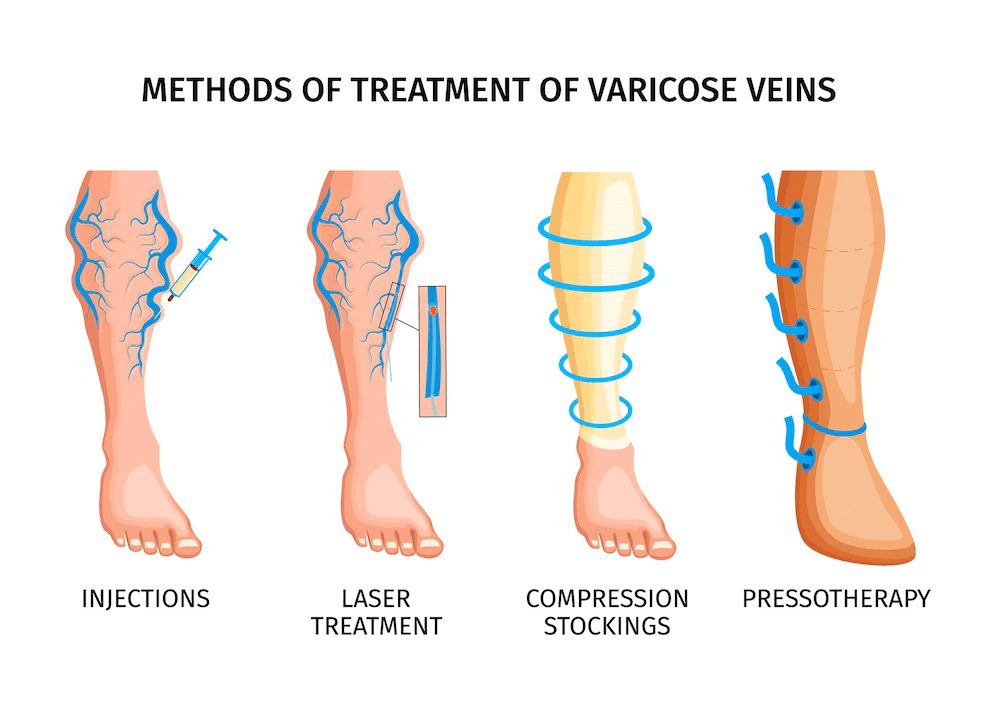
Effective Treatment Options for Varicose Veins: Seeking Professional Care
When natural remedies are not sufficient in managing varicose veins, various medical treatments can provide relief and improve the condition. It is essential to consult a healthcare professional for a proper evaluation and personalized treatment plan. Here are some effective treatment options for varicose veins:
- Sclerotherapy: This non-surgical procedure involves injecting a solution into the affected veins, causing them to collapse and fade away over time. Sclerotherapy is suitable for smaller varicose veins and spider veins.
- Endovenous Laser Treatment (EVLT): A minimally invasive procedure that uses laser energy to close off varicose veins. The laser heat damages the vein, causing it to collapse and eventually be reabsorbed by the body.
- Radiofrequency Ablation: Similar to EVLT, this treatment uses radiofrequency energy to heat and seal varicose veins. The damaged vein is gradually reabsorbed by the body, alleviating symptoms.
- Ambulatory Phlebectomy: This surgical procedure involves the removal of varicose veins through tiny incisions. It is typically performed for larger veins close to the skin’s surface.
- Laser and Intense Pulsed Light (IPL) Therapy: These treatments target spider veins using concentrated light energy, causing them to fade and eventually disappear.
- High Ligation and Vein Stripping: A surgical procedure in which the affected vein is tied off and removed through small incisions. This treatment is reserved for severe cases or when other methods have not been effective.
- Venous Catheter Procedures: These procedures involve the use of a catheter to heat or close off the affected vein. Examples include endovenous laser ablation (EVLA) and radiofrequency ablation (RFA).
The choice of treatment depends on the severity of the varicose veins, the patient’s overall health, and the healthcare professional’s recommendation. It is crucial to have a comprehensive evaluation and discuss the benefits, risks, and expected outcomes of each treatment option.
*Disclaimer: The information provided in this article is for educational purposes only and does not replace professional medical advice. If you are experiencing severe varicose vein symptoms or complications, it is essential to consult a qualified healthcare practitioner for an accurate diagnosis and appropriate treatment.
Author Information
Contributed by
Author Contribution: Reviewed by Dr. Ram Reddy, MD – General Physician, and Rajeshwar Rao, Pharm D.
