A disorder known as tachypnea causes the breathing rate to be elevated. Adults typically breathe between 12 and 20 times each minute. Numerous things, such as temperature, infection, anxiety, pain, and exertion, can result in tachypnea. Rapid, shallow breathing, chest pain, and shortness of breath are all signs of tachypnea. Tachypnea treatment often aims to treat both the underlying cause and the symptoms.
Adults normally breathe 12 to 20 times per minute while at rest, which is considered the normal respiratory rate. The normal range is typically higher in newborns and children due to their higher metabolic rates. Tachypnea is often described as a respiratory rate that is higher than what is considered normal for the age group in question.
Tachypnea may be a sign of a number of underlying diseases or physiological reactions. It frequently results from the body’s attempt to make up for a drop in oxygen or a rise in carbon dioxide levels. Tachypnea can be caused by illnesses such as respiratory infections, asthma, pneumonia, anxiety, heart failure, metabolic acidosis, and specific drugs.
The number of breaths per minute may increase when a person has tachypnea because their breathing may be shallow and quick. Shortness of breath, tightness in the chest, an accelerated heart rate, and weariness can all occur together with tachypnea.
If you suffer from tachypnea or are worried about your breathing, speaking with a medical expert is crucial. They are able to assess your ailment, ascertain the underlying reason, and create an effective treatment strategy.
Causes of Tachypnea
- Respiratory infections: Tachypnea is frequently observed in breathing-related conditions such as pneumonia, bronchiolitis, or influenza. The respiratory tract’s irritation brought on by these infections could accelerate breathing.
- Asthma: Asthma is a long-term respiratory disease marked by inflammation and airway constriction. Tachypnea can happen during an asthma attack as the body strives to make up for the reduced airflow.
- Chronic obstructive pulmonary disease (COPD): Emphysema and chronic bronchitis are two lung diseases that worsen over time. As a result of their lungs’ restricted airflow and resulting compensatory rapid breathing, people with COPD may have tachypnea.
- Anxiety and panic attacks: As a result of hyperventilation and intense feelings, anxiety, or panic attacks can result in tachypnea. People may breathe quickly and shallowly when under stress or terror, which increases their respiratory rate.
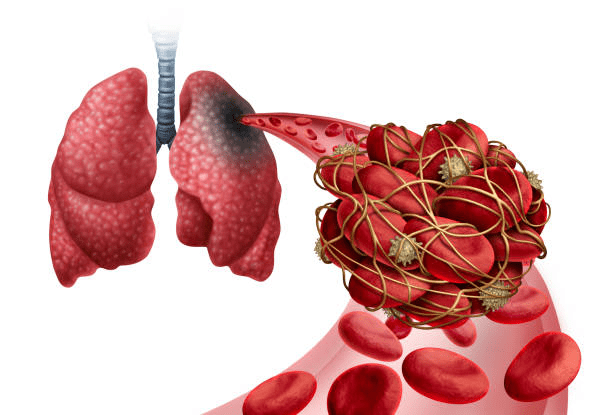
- Heart conditions: Tachypnea can be brought on by certain cardiovascular conditions, including pulmonary arterial disease and congestive heart failure. Increased respiratory efforts can be caused by a lack of oxygen as a result of the heart’s lower capacity to pump blood efficiently.
- Medication: Tachypnea is a side effect that can occur when using some drugs, including bronchodilators.
Symptoms of Tachypnea
- Shallow and fast breathing are the main signs and symptoms of tachypnea. Tachypnea is typically defined as an adult respiratory rate of breathing that is greater than 20 breaths per minute.
- Breathing difficulties or a sense of being out of breath can be brought on by tachypnea. With effort or exercise, this discomfort could get worse.
- A feeling of tightness or discomfort in the chest may be experienced by certain tachypneic as a result of their increased breathing effort.
- Rapid heartbeat: As the body strives to make up for the low oxygen levels or other underlying causes, tachypnea frequently comes with an elevated heart rate (tachycardia).
- Tachypnea is frequently related to shallow breathing, which is characterized by fast breathing that lacks inhalation and exhalation of sufficient depth.
- A feeling of being unable to catch one’s breath, anxiousness, or restlessness can be brought on by rapid breathing and shortness of breath symptoms.
- Exhaustion or tiredness may result from the greater effort of fast breathing.
- Cyanosis: In severe situations, tachypnea can lead to insufficient oxygenation, resulting in cyanosis, which is a bluish coloring of the skin, lips, or nail beds brought on by low oxygen levels.
The risk of Tachypnea
- Reduced gas exchange: Tachypnea can cause rapid breathing, leading to shallow, ineffective breaths that reduce the air that reaches the lungs. Hypoxemia and respiratory acidosis may result from insufficient oxygen intake and ineffective carbon dioxide removal.
- Respiratory distress: Tachypnea that is accompanied by rapid, labored breathing is a sign of respiratory distress. It could be an indication of serious respiratory illnesses such as acute respiratory distress syndrome (ARDS) or pulmonary edema, both of which call for prompt medical attention.
- Fatigue and tiredness: Prolonged tachypnea can cause fatigue and exhaustion since the respiratory muscles are using more energy. This may have an effect on general health and quality of life.
- Tachypnea frequently happens as a symptom of an underlying medical issue that is progressing. If the underlying reason is not addressed, it could get worse and cause more problems and health hazards.
Treatment for Tachypnea
- Oxygen therapy: To raise oxygen levels and relieve the symptoms of tachypnea in cases of severe hypoxemia or respiratory distress, supplementary oxygen may be given.
- Management of anxiety: If anxiety or panic attacks are the cause of tachypnea, anxiety-reduction strategies such as deep breathing exercises, relaxation techniques, or counseling may be used.
- Pulmonary rehabilitation: Programmes for pulmonary rehabilitation can aid in the improvement of lung function, the reduction of dyspnea, and the enhancement of general respiratory health in those with chronic respiratory illnesses like COPD.
- Modifications to one’s way of life: Living a healthy lifestyle, which includes getting regular exercise, quitting smoking, and eating a balanced diet, can improve respiratory health and help treat tachypnea brought on by long-term diseases.
Prevention of Tachypnea
- Routine medical examinations: It’s critical to regularly have medical tests in order to identify and treat any underlying medical disorders that may be causing your tachypnea early on. The identification and management of potential risk factors might be aided by routine visits to your healthcare provider.
- Manage underlying medical conditions: If you have any pre-existing conditions like asthma, chronic obstructive pulmonary disease (COPD), heart disease, or anxiety, it’s important to work closely with your healthcare practitioner to manage and treat these conditions. The likelihood of experiencing tachypnea episodes might be decreased with proper management.
- Identify and stay away from factors that could cause episodes of fast breathing. Consider the importance of avoiding known allergens or irritants that might cause respiratory distress if you have asthma.
- Manage your stress: Tachypnea episodes can be impacted by worry and anxiety. It is possible to lessen the frequency and severity of fast breathing episodes by implementing stress-reduction strategies including deep breathing exercises, meditation, yoga, or relaxing hobbies and pastimes.
- Maintain a healthy lifestyle: Living a healthy lifestyle helps keep your respiratory system in good shape. This entails keeping a healthy weight, exercising frequently, abstaining from smoking and passive smoking, and limiting the use of sedatives and alcohol as these substances might impair respiratory function.
- Diaphragmatic breathing is one of the right breathing strategies that can be learned and practiced to increase respiratory efficiency and lessen the risk of tachypnea.
Complications of Tachypnea
- Respiratory distress is a condition in which a person has trouble breathing and feels out of breath. Tachypnea can induce this. Excessive breathing effort and exhaustion may result from this.
- The condition known as hyperventilation syndrome can result from persistent or severe tachypnea. Rapid, deep breathing is a defining feature, and it raises the risk of an improper oxygen-to-carbon dioxide blood ratio. Lightheadedness, dizziness, numbness or tingling, and chest pain are some of the symptoms that may result from this.
- Respiratory alkalosis: Tachypnea-related hyperventilation can cause this condition, which causes the body to become more alkaline due to an imbalance in the pH levels. Confusion, twitching, and tingling feelings are a few signs that could result from this.
- Tachypnea can put more strain on the heart and circulatory system, which can lead to cardiovascular issues. As a result, there may be potential problems like increased heart rate, increased cardiac workload, arrhythmias (abnormal heart rhythms), palpitations, and a higher risk of heart failure.
- Oxygen deprivation: Breathing too quickly can cause shallow breaths that may not exchange enough oxygen. This may result in lower oxygen levels in the blood and tissues, which may harm dysfunctional organs.
- Fatigue and tiredness: Rapid breathing necessitates more effort, which can result in fatigue and exhaustion. This may have an effect on everyday tasks and general quality of life.
- Effect on underlying illnesses: Asthma, chronic obstructive pulmonary disease (COPD), and congestive heart failure are a few respiratory conditions that tachypnea can make worse. It can exacerbate symptoms, cause respiratory distress, and raise the chance of complications from these diseases.

Natural remedies for Tachypnea
The body can be calmed and the pace of breathing can be slowed down by engaging in relaxation techniques such as deep breathing exercises, meditation, or yoga. These methods work to calm the body and mind, which may help with symptoms of tachypnea.
Positioning yourself correctly and maintaining an upright posture will help you breathe easier. You can help to open up your airways and make breathing easier by sitting up straight or elevating yourself with cushions while lying down.
Warm liquids: Consuming warm liquids, including herbal teas or warm water, can aid in respiratory system sedation and relaxation. In order to facilitate its excretion, it may also help thin mucus.
Humidification: Adding moisture to the air using a humidifier or a steamy shower can help relieve respiratory symptoms and improve breathing comfort.
Maintain proper hydration: Respiratory health can be maintained by maintaining proper hydration. Make sure you consume enough water throughout the day to maintain the moisture in your airways and avoid respiratory discomfort.
Avoid triggers: If you’ve discovered any triggers, such allergies or pollutants, that make your tachypnea worse, attempt to limit your exposure to them. This can entail staying away from specific settings, donning a mask, or using air purifiers.
Diagnosis of Tachypnea
- Medical history: The healthcare professional will start by gathering information about your symptoms, their frequency and intensity, any underlying illnesses you may have, and any potential causes or triggers for your episodes of rapid breathing.
- Physical examination: The respiratory system will be the primary focus of a thorough physical examination. Your breathing effort, pattern, and rate will all be evaluated by the medical professional, who will also listen to your lungs for any unusual noises.
- Measurement of respiratory rate: The respiratory rate will be assessed to see if it is within the range of tachypnea. Tachypnea is typically defined as an adult respiratory rate of breathing that is greater than 20 breaths per minute.
- Diagnostic tests: The healthcare provider may suggest additional tests to assist determine the underlying cause of tachypnea based on the results of the history and physical examination. These tests could consist of:
- Blood tests: Blood tests can reveal details about blood pH, oxygen and carbon dioxide levels, and other markers that could point to disorders in the respiratory or metabolic systems.
- Chest X-ray: To evaluate the health of the lungs, spot any anomalies, or rule out specific respiratory disorders, a chest X-ray may be prescribed.
- Tests measuring lung capacity and function are known as pulmonary function tests, and they are used to assess breathing effectiveness and find any underlying respiratory disorders.
- Electrocardiogram (ECG): An ECG can be used to evaluate the electrical activity of the heart and find any anomalies that might be causing tachypnea.
- Imaging tests: To assess the respiratory system’s structural components or find any underlying disorders, additional imaging tests like a CT scan or MRI may be advised in some circumstances.
*Disclaimer: This article is for informational purposes only and should not substitute professional medical advice. Please consult a healthcare professional for a thorough evaluation of your symptoms and appropriate treatment.
